DR.MOHAN GIRI, DR.RACHNA GOENKA
ABSTRACT: – Hypertension is an “iceberg” disease. It is evident that only about half of the hypertensive people are aware of the condition, about half of those aware of the problem are being treated and only about 50% of those treated are considered adequately treated. Till today the measurement of pulse and blood pressure are not always taken as a routine work by professional’s thereby missing serious disease diagnosis like ‘Hypertension’. This article will help professionals to overcome such problems and consider the seriousness of the facts even in homoeopathic practice.
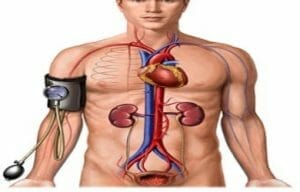
INTRODUCTION: – Hypertension is a chronic condition of concern due to its role in the causation of coronary heart disease, stroke and other vascular complications. It is the commonest thread posing a major public health challenge to population in socioeconomic and epidemiological transition, which accounts for 20-50% of all death.
Definition of hypertension is difficult and by necessity arbitrary. There is also a direct relation between cardiovascular risk and blood pressure, rise of which increases the risk of both stroke and coronary events.
As intervention trials include only adults aged 18 years or older, the definition and classification of hypertension refer to adults not taking antihypertensive drugs and not actually ill, and based on the average of two or more occasions after initial screening. The table below shows the classification of hypertension on the basis of blood pressure level.
| CATEGORY | SYSTOLIC BLOOD PRESSURE (in mm of Hg) | DIASTOLIC BLOOD PRESSURE( in mm Hg) |
| Normal | <130 | <85 |
| High Normal | 130-139 | 85-90 |
| HypertensionStage 1 (mild)
Stage 2 ( moderate) Stage 3 (sever) |
140-159
160-179 >180 |
90-99
100-109 >110 |
When systolic and diastolic blood pressure falls into different categories, the higher category should be selected to classify the individual’s blood pressure.
The world health organization (WHO) criterion for the definition of hypertension is-“Persistent rise of basal blood pressure that is measured at complete physical and mental rest that is more than 150/90 mm of Hg in an adult.”
Isolated systolic hypertension is defined as a systolic blood pressure of 140 mm of Hg or more and a diastolic blood pressure of less than 90 mm of Hg”.
Persistent fall of basal blood pressure less than 100/50 is considered as hypotension.
MEASUREMENT OF BLOOD PRESSURE
Blood Pressure can be defined as the product of cardiac output and peripheral resistance; or the lateral pressure exerted by the column of blood in the vessels during each ventricular contraction. The peripheral resistance depends upon;-
- Velocity of blood (directly proportional to peripheral resistance):- Velocity of blood increase in any fever, severe anaemia, thyrotoxicosis and in pregnancy etc.
- Viscosity of Blood (directly proportional to peripheral resistance):- Viscosity of blood increases in Polycythemia Vera
- Elasticity of vessel wall (universally proportional to peripheral resistance):- Elasticity of vessel wall decreases in atherosclerosis.
- Lumen of vessel (universally proportional to peripheral resistance):-Lumen of vessel wall decreases in Pheochromocytoma.
Process of examination: –
- The blood pressure instrument should be placed at a leveled surface at about the level of heart.
- Scale of the instrument should be at the level of the observer’s eyes.
- Patients should be at maximum mental and physical rest and sufficient time is to be allowed to recover from any recent exercise or emotional upset for which at least half an hour rest is given.
- Blood pressure is measured either in sitting or lying down positions.
- The upper arm is relaxed, extended and comfortably laid by the side of body. The arm is kept bare up to the shoulder.
- Width of the cuff should be 5” or 12 cm (in adult), 1”- 2” (in children) and 1” for infant while the length should be not less than 25 cm.
Application of cuff:-
- Cuff should be applied when fully deflected.
- The middle of the cuff from where two tubes come out should be on medial side.
- The lower border of the cuff should be applied 2-5 cm above the cubital fossa.
- The cuff should be close to the skin, neither loose nor folded.
Method of Noting Blood Pressure: –
A few salient points need to be mentioned about measuring blood pressure. A WHO study recommended the sitting position than the supine position for recording blood pressure. In any clinic a uniform policy should be adopted, using either the right or left arm consistently.
There are certain indirect methods of recording the blood pressure. They are as follows:-
- Palpatory method
- Ascultatory method
- Flush method – used mainly in infants
- Oscillatory method.
- Other methods like ultrasonic and tomometry methods.
In clinical practice both palpatory and auscultatory methods at the same time are applied for better, easy and accurate recording.
Techniques; –
Slow rise of Hg level where the rise of pressure should be at the rate of 10mm of Hg. Bronchial artery is first palpated and then chest piece of stethoscope is placed lightly and accurately over it. After raising the pressure for about 30mm of Hg above the level of systolic pressure by palpatory method, the pressure is gradually reduced at the rate of 3mm of Hg per second and the findings are noted.
Phase I: – Highest point at which successive sounds are heard, become faint and tapping, thereafter growing louder—is systolic pressure by ascultatory method.
Phase II: – On further reduction of pressure there appears a phase of murmur, which is of short period and sometimes may be absent.
Phase III: – Clear and loudest phase of auscultative finding appears.
Phase IV: – Sound suddenly become dull and muffled– considered as diastolic pressure (by Korotkoff’s).
Phase V: – Highest level at which sound disappears completely is considered as the diastolic pressure by auscultation as per modern concept.
The systolic and diastolic pressures should be measured at least three times over a period of at least three minutes and the lowest reading recorded. For reasons of comparability, the data should be recorded everywhere in a uniform way. The ideal time for recording the blood pressure is early in the morning after awakening from sleep but not while still lying in bed.
Despite more than hundred years of experience with the measurement of blood pressure, discussion continues about its reliability and wide variability in individual subjects. Accurate measurements are essential under standardized condition for valid comparison between persons or group over time.
Three sources of errors have been identified in the recording of blood pressure. They are:-
- Observer Errors i.e. hearing acuity.
- Instrumental Errors i.e. leaking valve, and cuffs that do not encircle the arm properly.
- Subjects Errors i.e. the circumstances of examination. These include the physical environment, the position of the subject, external stimuli such as fear and anxiety etc.
CLASSIFICATION OF HYPERTENSION
On the basis of aetiological involvement hypertension can be classified into the following categories:-
- Primary or Idiopathic: due to almost unknown aetiology which may be further categorised into:-
- i) Essential hypertension: – This may be of two types:
(a) Benign: – This is a most common type of hypertension which mainly occurs due to familiar condition i.e. if both the parents are sufferers, chances are higher.
(b) Malignant: – This occurs due to an untreated case of benign hypertension.
- ii) Toxaemia of pregnancy:-This is also considered as an essential hypertension.
- Secondary Hypertension; – This occurs mainly below the age of 30 years and may be due to the under lying causes:
- Renal Causes:–
- Acute glomerulonephritis
- Chronic glomerulonephritis
- Chronic pyelonephritis
- Polycystic kidney
- Renal tumour
- Renal artery stenosis
- Endocrinological Causes:–
- Thyrotoxicosis
- Cushing’s syndrome
- Pheochromocytoma
- Conn’s syndrome
- Neurological Causes:-
- Cerebral tumour
- Pseudo bulbar palsy
- Bulbar poliomyelitis
- Cerebro-Vascular Disease
- Metabolic Causes:-
- Diabetes Mellitus
- Chronic Gout
- Atherosclerosis
- Iatrogenic Causes:-
- Use of oral contraceptives pills
- Prolonged steroid therapy i.e. in bronchial asthma
- Miscellaneous Causes:-
- Coarctation of aorta
- Psychogenic
- SLE
- Polyarteritis nodosa
Homoeopathic concepts regarding the aetiology of hypertension include certain predisposing factors which are responsible for the disease condition. It makes an individual susceptible to a disease process. It consists of accessory circumstances and genetic predisposition which is impregnated with the chronic miasmatic dyscrasia as psoric, sycotic and syphilitic. The pathology and clinical features will depend on the dominating miasmatic state of the patients.
CLINICAL FEATURES OF HYPERTENSION
The symptoms of hypertension are usually variable and at times very vague. There may be no symptoms and the disease may be diagnosed accidentally during routine examination.
Due to a wide range of variability of clinical features of hypertension, it can be categorized into three stages:-
- Hypertension: – This may be mainly asymptomatic.
- Hypertensive disease: – During the attacks the symptoms are usually psychogenic but some common symptoms are also present such as:
- Headache, often occipital and occurring in the morning
- Easy fatigability
- Insomnia
- Lack of concentration
- Loss of memory
- Breathlessness
- Occasional palpitation.
- Hypertensive disease with complications:-At a later stage as different target organs of the body are involved, various additional sign and symptoms may develop usually as a part and parcel of complication. The main target organs are heart, brain, kidney and eyes.
This occurs mainly secondarily due to involvement of the target organs and usually manifested by apparent signs such as:
- i) Flushing of face
- ii) Blood pressure > 150 / 90 mm of Hg and even more
iii) Pulse – mainly slow
- iv) Ophthalmoscopic Examination: – There will be retinopathy especially in chronic and malignant hypertension which has the following grades-
- Grade I – Thickening of wall of retinal artery and arterioles known as “silver wiring” of retinal artery and arterioles.
- Grade II – There will be further thickening which leads to arterio-venous nipping resulting in compression of vein by artery.
- Grade III – In addition to Grade I and Grade II, there may be haemorrhage and production of exudates known as ‘cotton-wool exudates’.
- Grade IV – Palpilloedema with or without Grade I to Grade III changes.
- v) There may be palpable kidney due to malignant hypertension
COMPLICATIONS OF HYPERTENSION
| Acute Complications | Chronic Complications |
|
|
|
|
|
|
|
|
|
PROGNOSIS OF HYPERTENSION
The prognosis of hypertension depends on the following factors i.e:
- Degree of hypertension
- Response to therapy
- Degree of ECG changes
- History of paroxysmal nocturnal dyspnoea and cardiac failure
- Ocular changes
- Degree of cardiac decompensation
LABORATORY INVESTIGATION OF HYPERTENTION
Routine investigation of the hypertensive patient should include:
- Chest X-ray
- ECG
- Echocardiogram
- Urinalysis
- Fasting blood for lipids and glucose
- Serum urea, creatinine and electrolytes
If the urea or creatinine is elevated, more specific renal investigations are indicated such as: creatinine clearance, renal ultrasound and renal isotope scans. Low serum potassium may indicate an endocrine disorder, and aldosterone, cortisol and rennin measurements must then be made.
Clinical suspicion of phaeochromocytoma should be investigated further with measurement of urinary metanephrines and plasma catecholamine.
ECG may show evidence of coronary artery disease or left ventricular hypertrophy, although echocardiography is a far more sensitive method for detection of left ventricular hypertrophy.
The chest X-ray may show cardiomegaly or pulmonary congestion if heart failure is developing. Rib notching on the X-ray may be a sign of coarctation of the aorta and should be investigated further with an MRI scan.
MANAGEMENT OF HYPERTENSION
Unless the patient has severe or malignant hypertension, there should be a period of assessment. During the assessment period secondary causes of hypertension should be excluded, the target organ effect of hypertension should be evaluated, and any concomitant conditions (e.g.dyslipidaemia or diabetes) identified. The assessment period is in three stages-
- Repeated blood pressure measurement combined with advice
- Non pharmacological treatment
- Medicinal / pharmacological treatment
- Non pharmacological treatment and management depends upon the lifestyle modification and identification of risk factors. Hypertension is not only one of the major risk factors for most forms of cardiovascular disease, but it is a condition with its own risk factors. WHO has recently reviewed the risk factors for essential hypertension? These may be classified as:
- Non-modifiable risk factors:
(a). AGE:-Blood pressure rises with age in both sexes and the rise is greater in those with higher initial blood pressure. Age probably represents an accumulation of environmental influences and the effects of genetically programmed senescence in body systems.
(b). SEX:- Early in life there is little evidence of a difference in blood pressure between the sexes. However, at adolescence men display a higher average level. This difference is most evident in young and Middle Ages adults. Late in life the difference narrows and the pattern may even be reversed. Post-menopausal changes in women may be the contributor factor for this change.
(c). GENETIC FACTORS:- There is considerable evidence that blood pressure levels are determined in part by genetic factors, and that the inheritance is polygenic. The evidence is based on twin and family studies Twin studies have confirmed the importance of genetic factors in hypertension. The blood pressure values of monozygotic twins are usually more strongly correlated than those of zygotic twins. In contrast, no significant correlation has been noted between husband and wives, and between adopted children and their adoptive parents.
Family studies have shown that the children of two normotensive parents have 3 percent possibility of developing hypertension, whereas this possibility is 45% in children of two hypertensive parents. Blood pressure level among first degree adult relatives has also been noted to be statistically significant.
Attempts to find genetic markers that are associated with hypertension have been largely unsuccessful. The detailed mechanism of heredity i.e., how many genes and loci are involved and their mode of inheritance have not yet been conclusively elucidated.
(d). ETHNICITY: – Population studies have consistently revealed higher blood pressure level in black communities than other ethnic groups. Average difference in blood pressure between the two groups varies from slightly less than 5 mm Hg during the second decade of life to nearly 20mm Hg during the sixth. Black Americans of African origin have been demonstrated to higher blood pressure levels than whites.
- Modifiable risk factors:
(a). Obesity: – Reduction of weight in an obese person should be promoted. Over-weight has been seen in epidemiological studies to be an important risk factor for higher blood pressure, and there seem to be a linear relation between body weight and blood pressure. Clinical trials have shown that weight loss, especially when combined with dietary sodium restriction, lowers blood pressure in hypertensive and also in normotensive patients.
It is therefore important that all patients be advised to maintain weight near optimal by reducing calorie intake and increasing physical activity. Since sustained weight reduction is difficult to achieve, prevention of weight gain should be emphasized.
(b). Salt intake: – Dietary salt intake has a linear association with blood pressure. Reduced sodium intake to approximately 100mmol per day can prevent hypertension, can facilitate blood pressure control in elderly patients on medication and can potentially prevent cardiovascular events in overweight individuals. The data from these led to current recommendations to limit salt intake to 6 grams per day.
To reduce salt intake, individuals should consume food s low in salt and limit the amount of salt added to food. Food rich in salt, like pickles, processed food s, chips and chutneys, should be avoided.
(c). Alcohol Consumption: – Over consumption of alcohol has both chronic and acute deleterious effect on blood pressure. The relationship between high alcohol intake (typically three or more drinks per day) and elevated blood pressure has been documented in many epidemiologic studies.
The several studies recommends that alcohol intake should be no more than two drinks per day by men and one drink per day by women among those who drink. In view of other health benefits, alcohol consumption is not recommended for nondrinkers.
(d). Physical activity:- Regular exercise programs should be encouraged. Increasing aerobic physical activity such as brisk walking, jagging, swimming or bicycling has been shown to lower blood pressure. Significantly, this reduction is independent of any concomitant weight loss.
Physical activity has been shown to reduce systemic vascular resistance, most likely due to a decrease in the activity of the sympathetic nervous system. This is evidenced by lower plasma nor epinephrine levels in exercising indisuals compare to sedentary ones and also there is a decrease in plasma rennin activity. It is recommended that persons exercise for at least 30 minutes on most, if not all, days of the week.
(e). Other factors:-
(i) Saturated fat: Restriction of cholesterol (prefer vegetable oil instead of animal oil)
(ii) Dietary fiber: Several studies indicate that the risk of chronic heart disease and hypertension is inversely related to the consumption of dietary fiber.
(iii) Socio-economic status: Smoking and psychological factors should be avoided
(iv) Hyperlipidimic patients should be treated accordingly and renal and endocrinal disease should be managed properly.
(v) Behavioral techniques, meditation and yoga should be promoted.
All these factors are considered as modifiable risk factors by WHO, because just modifying these can control a vast majority of hypertensive cases.
- Pharmacological treatment and management: The decision to commence drug therapy should usually be made only after a careful period of assessment. The aim of drug treatment is to reduce the risk of complication of hypertension which should be carefully explained to the patients.
- A. Individual Drug Response Approach: Homoeopathic treatment depends upon the symptom syndromes of the disease condition and individual character of the patients. As the disease is severe and related to severe complications, its management is also essential. There are certain drugs which may be helpful for the management of cases of hypertension with or without constitutional medicines depending upon the nature and degree of disease condition such as:
- i) Natrum Muriaticum-Tachycardia with intermittent pulse < when lying down. Fluttering palpitation which shakes the whole body. This drug is recommended as the best remedy in high potency for essential hypertension where taking too much salt is the main etiological factor.
- ii) Rauwolfia Serpentina-This is known as a general remedy for hypertension. The recommended physiological dose is 10-20 drops three to four time a day as per necessity. This drug is more beneficial for systolic hypertension than the diastolic one. This drug is recommended as the best remedy for systolic hypertension where anxiety is the main aetiological factor.
iii) Convallaria Majalis– Palpitation from least exertion. Tobacco heart especially due to cigarette smoking. Hypertension with marked dyspnoea especially orthopnoea. This drug is recommended as the best remedy for diastolic hypertension where secondary cause is the main aetiological factor. From usual practice it has been found that this drug is effective in the cases of malignant diastolic hypertension even when the patient is taking modern antihypertensive drugs without satisfactory response (further research required).
iv) Baryta Muriatica– This drug is highly effective in systolic hypertension where arterio-sclerosis is the main aetiological factor. Increased tension of pulse where a high systolic pressure with a comparatively low diastolic pressure is attended with cerebral and cardiac symptoms.
v) Aurum Metallicum– Palpitation with rapid pulse. Hypertension due to arterio-sclerosis. According to William Boerick 30 potency is quite effective.
vi) Uranium Nitricum– Hypertension with degeneration of vital organs like liver and kidney. This drug is said to be effective in cases of diabetic nephropathy and hypertension. The therapeutic keynote symptoms are great emaciation, debility and tendency to ascites with general dropsy.
vii) Lycopus Verginicus – Lowers the blood pressure, reduces the rate of heart and increases the length of systole to a great degree. From usual practice it has been found that this drug is effective in cases of thyrotoxicosis where pulse pressure is high and heart action is rapid, in physiological dose (further research required).
- Repertorial Approach: Repertory is the dictionary of the homoeopathic literature where symptoms of materia medica arranged in a systemic way along with indicated medicines, and hypertension is the clinical condition occurring due to several underlying causes which may be manifested by several signs and symptoms as per their organic evolvement.
In homoeopathic literature several author of repertory has included hypertension as a direct rubrics in Generalities chapter and in other chapters also which may be controversial at the time with our philosophy, still we are coating the some important rubrics and authors for the professionals benefit if they can adopt.
i). Synthesis Repertory; This repertory is based on RADAR Software and compiled by Dr.Frederich Schroyen’s. As per Kentian philosophy there are general rubrics with drugs followed by sub rubrics and sub-sub rubrics with related drugs of hypertension which are as follows-
- –Apoplexy; accompanied with: Glon, Op.
- –Diabetes Mellitus; accompanied by: Sec.
- –Dialysis from: Acon-f,adren, Ser-ang.
- –Excessive: Toxo-g.
- –hypertrophy; heart of from: Cratag.
- –Lung complaints after: Nat-ox-acet.
- –Nephrosis; accompanied by: Fuma acid.
- –Nervous mechanism due to disturbed:Aur. M. N.
- –Urine; albuminous: visc.
- –Sudden-Adren,coffea.
ii). Concise Repertory of Homoeopathic Medicines by R S Phatak , threre is direct rubrics as Blood Pressure-High and list of some drugs and then sub rubrics as
- –diastolic low, and –Bar-Mur.
- –Sudden rise of- Coffea.
As per homoeopathic philosophy any drug can be indicative for the case depending upon the totality of symptoms, but those listed above have been given on the basis of personal work experience and research which may be helpful for the professional discipline.
BIBLIOGRAPHY
- Park.K.Park.’s Textbook of “Preventive and Social Medicine”.18th Edition.p.p.293-298.
- WHO (1996).ATechnRep.NO.862.
- Hart, JT (1980).Hypertension. Library of General Practitioner Series by Churchill Livingstone.
- Kumar and Clark, Clinical Medicine, Systemic Hypertension; 5th edit, p.p.729-736.
- British Hypertension Society Working Party (1993).Management guidelines in essential hypertension report of the second working party. British Medical Journal 306:983-987.
- Swales JD (1994). Textbook of Hypertension. Oxford: Blackwell Scientific.
- Boericke W. Pocket Manual of Homoeopathic Materia Medica & Repertory; B. Jain Publishers (P) Ltd. New Delhi. Reprint edit, 1994.
- Hahnemann S.Organon of Medicine, B. Jain Publishers (P) Ltd, New Delhi.1970.
- Dr.Schroyens’s Frederik.The Essential Synthesis (9.2E); Homoeopathic Book Publishers, London. Oct 2007, PP-1872.
- Dr.Phatak S K. A Concise Repertory of Homoeopathic Medicines-Alphabetically arranged; B. Jain Publishers (P) Ltd. New Delhi. June 2000, PP 38.
- Bhatt SP, Luqman-Arafath TK, Guleria R. Non-pharmacological management of hypertension. Indian J Med Sci 2007; 61:616-24.
ABOUT THE AUTHORS
- Dr.Mohan Giri has done B.Sc (Hons) in bio-sciences from Varanasi and then BHMS (Hons) and M.D.(HOM) both from NIH, Kolkata. Thereafter he has worked as a Research Fellow at NIH and published several articles in different journals like CCRH Bulletin and Indian Journal of Physiology and allied Science, New Delhi and then NIH Bulletin and in National Homoeo Recorder. He worked as Lecturer in NSHMCH Bhopal. At present he is working as a Lecturer in the Department of Practice of Medicine at Mahesh Bhattacharyya Homoeopathic Medical College & Hospital Howrah (Govt of West Bengal).
- Dr. Rachna Goenka has completed her B.H.M.S. (Hons) from The Calcutta Homoeopathic Medical College and Hospital. Currently she is working as a Lecturer in the Department of Homoeopathic Pharmacy at Mahesh Bhattacharyya Homoeopathic Medical College and Hospital, Howrah (Govt. of West Bengal).

excitable italians with their garlic and onion rarely have hypertension,these are words of elizabeth wright hubbard left in her writing in homoeorecorder article relation diet and homeopathic remedies.cider raw apple help arthritic patient.soda is alkaline but acidity producer replace by lemon citrus juice.improve colon flora by buttermilk.honey a formic acid and raddish anti uric acid.homeo remedies enable person to have natural assimilation from food.detoxify liver by adding lemon juice to white of egg.red clover tea useful cancer patients.such buried articles modern dieticians think are childish knowledge.reduce weight of fatty by garcinia cambodian grass make a person shun every food and imprint permanent disease.